The integrity of government-administered healthcare hinges on a foundational yet frequently underestimated pillar: claims management and assurance systems. As public health programs expand globally from the United States' Medicare and Medicaid to India's Ayushman Bharat and the United Kingdom's National Health Service, the mechanisms by which claims are submitted, adjudicated, and reconciled have become critical barometers of system efficacy, fiscal responsibility, and citizen confidence.
The Scale of the Challenge
Government healthcare authorities face unprecedented complexity in claims oversight. Consider the magnitude: Medicare alone processes over one billion claims annually, while India's Ayushman Bharat, the world's largest government health insurance program, manages coverage for over 500 million beneficiaries. Within this vast ecosystem, the statistics reveal systemic vulnerabilities that demand urgent attention.
Industry analyses indicate that 15-25% of medical claims are initially denied or rejected, with an alarming 65% never resubmitted, representing substantial resource losses to publicly-funded healthcare providers. These figures transcend mere budgetary concerns. They represent diverted resources that could otherwise expand coverage, improve care quality, or reduce taxpayer burden.
.jpg)
Essential Strategies for Government Healthcare Authorities
Based on international best practices and emerging technological capabilities, government healthcare administrators should prioritize the following strategic imperatives:
Implement Comprehensive Audit Infrastructure: Government claims systems must incorporate immutable audit trails with time-stamped documentation of every transaction. Regular internal and external audits conducted by independent bodies should verify compliance with coding standards, payment rules, and data protection protocols. Transparency mechanisms, including public dashboards displaying aggregated claims metrics, denial rates, and processing times, enhance public accountability and enable informed policy adjustments.
Deploy AI for Fraud Detection and Prevention: Machine Learning (ML) algorithms can analyze vast historical datasets to identify irregular patterns indicative of fraud, waste, or abuse. Government authorities should invest in AI tools that flag anomalous claims before payment authorization, reducing both financial losses and administrative burden. Research indicates that AI implementation can reduce denial rates by approximately 30% while increasing first-pass claim acceptance by 25%, representing substantial efficiency gains for public systems.
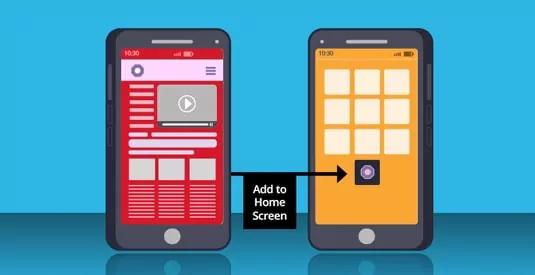
Establish Interoperable, Integrated Digital Platforms: Fragmented legacy systems create data silos that undermine efficiency and oversight. Government healthcare authorities must transition towards unified, cloud-based revenue cycle management platforms that integrate with electronic health records, automate eligibility verification, and provide real-time compliance checking. Such integration enables immediate identification of errors and inconsistencies, preventing denials and reducing the administrative cost per manually processed claim.
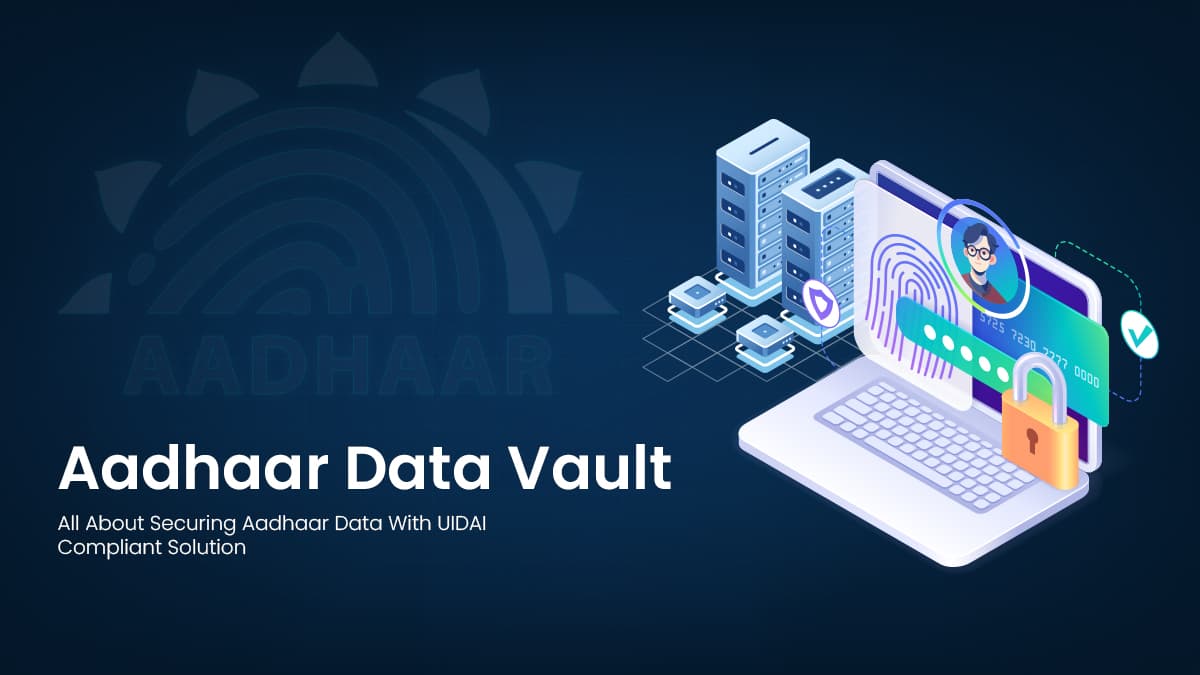
Ensure Rigorous Regulatory Compliance: Government claims systems must exemplify adherence to data protection regulations, including HIPAA standards in the United States, GDPR requirements in the European Union and DPDP in India. This encompasses encryption protocols, role-based access controls, breach notification procedures, and regular security audits. Compliance is not merely legal obligation; it is the foundation of citizen trust in government stewardship of sensitive health information.
Strengthen Cybersecurity Resilience: Government authorities must implement multi-layered security architectures, including intrusion detection systems, regular penetration testing, redundant processing capabilities, and comprehensive disaster recovery protocols. Public health systems cannot afford single points of failure in claims processing.
Foster Transparency and Stakeholder Engagement: Citizens deserve clear, comprehensible explanations of benefits and accessible mechanisms to question or appeal claims decisions. Government healthcare programs should provide online portals for claim tracking, establish patient advocacy services to assist with appeals, and publish regular performance reports. Transparency builds legitimacy; opacity breeds suspicion.
.jpg)
Scaling Impact in Public Health with CSM’s solution
At CSM Technologies, we understand that efficient claims administration is the backbone of sustainable, equitable healthcare delivery. Our Claim & Assurance Management System (CAMS) is engineered as a unified, end-to-end digital backbone that transforms the entire claims lifecycle - from pre-authorization to settlement into a seamless, transparent, and intelligently governed process.
CAMS brings together multiple mission-critical functions into a single, integrated platform. Its robust automation engine validates claims, minimizes manual intervention, and sharply reduces delays, errors, and leakages. The pre-authorization module ensures real-time, rule-based approvals for high-value procedures, while the Transaction Management System captures every treatment detail, from beneficiary information to discharge summaries, ensuring precision and traceability.
What sets CSM’s solution apart is its strong focus on governance and fraud control. With embedded fraud-mitigation checks, hospital empanelment workflows, mobile-based inspections, chatbot-driven beneficiary support, and a fully automated grievance redressal system, CAMS delivers unmatched oversight. The analytical dashboards empower authorities with real-time insights for faster decision-making and tighter financial control.
CSM’s deployment in Odisha's healthcare scheme demonstrates measurable excellence: over 1.2 million beneficiaries served across 838 empanelled hospitals, processing transactions exceeding Rs 480 crore. These metrics reflect not simply financial throughput but operational maturity - the system's capacity to maintain integrity, transparency, and efficiency under real-world demands. Our digital claims system stands as a powerful catalyst for Universal Health Coverage. It elevates efficiency, strengthens accountability, and ensures that public health schemes deliver maximum value where it matters most- to the last-mile beneficiary.
The Path Forward: Governance as Guarantor
The future of government healthcare claims management lies in transforming reactive oversight into predictive governance. Blockchain technology, with its capacity for immutable, transparent record-keeping, represents one promising frontier. Several government healthcare programs are exploring distributed ledger systems that would create shared, tamper-proof claims records accessible to authorized providers, payers, and regulators, fundamentally reducing reconciliation disputes and enhancing trust.
Equally important is cultivating a culture of continuous improvement within government healthcare agencies. This requires ongoing staff training on evolving regulations and coding standards, investment in analytics capabilities, and establishment of cross-functional governance committees that bring together clinical, financial, technical, and policy expertise.
The public trust is not given - it is earned through proven competence, unwavering accountability, and systems architected for integrity. Government healthcare authorities must lead this transformation, not follow it.












.jpg)

























We will verify and publish your comment soon.